Tocilizumab Plus Prednisone Taper Achieves Sustained Remission in Giant Cell Arteritis
12/04/2023
A 52-week regimen of tocilizumab combined with an 8-week prednisone taper achieved sustained remission among a majority of patients with giant cell arteritis (GCA), suggesting potential efficacy for reducing glucocorticoid exposure and associated toxicity, according to study results published in Lancet Rheumatology.
Giant cell arteritis is the most prevalent form of primary vasculitis, occurring most often in patients aged at least 50 years. Traditionally, glucocorticoids are the main treatment modality for controlling the disease. However, a substantial number of patients experience adverse events (AEs). With recent phase 3 clinical trials of tocilizumab demonstrating benefits in terms of GCA remission, researchers conducted a pilot trial to evaluate the efficacy and safety of tocilizumab in combination with prednisone among patients with GCA.
Researchers conducted a single-center, prospective, single-arm, open-label trial, including participants aged at least 50 years with either new-onset or relapsing GCA.
All patients received 162 mg tocilizumab in weekly subcutaneous injections for a total duration of 52 weeks; in addition to tocilizumab, all patients underwent a prespecified 8-week prednisone taper, with the initial prednisone dose ranging from 20 mg to 60 mg.
“
Such a strategy could obviate the need for and prevent many of the complications associated with long-term glucocorticoid use.
The primary study outcome was sustained prednisone-free remission at week 52, with criteria including achievement of normal erythrocyte sedimentation rates (<40 mm/h) and C-reactive protein levels (<10 mg/L). Secondary outcomes included the proportion of patients in remission at week 24, number of relapses, relapse rate, and glucocorticoid toxicity.
A total of 30 patients with GCA were enrolled in the study (60% women; 100% White; mean age, 73.7 years); 50% of patients had newly diagnosed disease and the remaining 50% had relapsing disease.
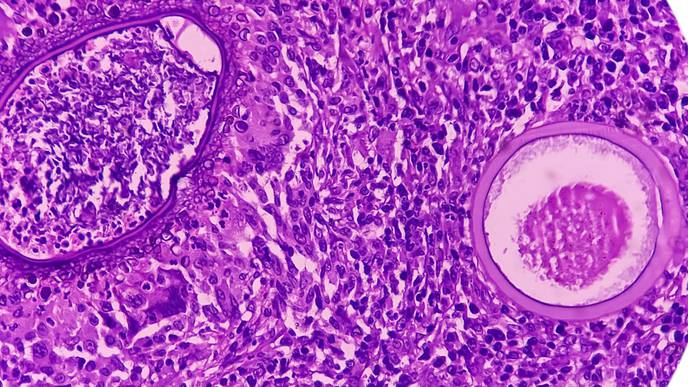
Giant cell arteritis was confirmed by temporal artery biopsy in 77% of patients and by vascular imaging in 47%. Clinical manifestations at baseline included cranial symptoms in 87% of patients and polymyalgia rheumatica symptoms in 57%.
Sustained prednisone-free remission at week 52 was achieved by 77% of patients.
Seven patients (23%) experienced a relapse after a mean period of 15.8 weeks. Relapses occurred among patients with both new-onset (5 patients) and relapsing (2 patients) disease. The mean annualized relapse rate for the entire cohort was 0.46 and the mean daily prednisone dose at the time of relapse was 2.1 mg.
Notably, the mean cumulative prednisone dose at week 52 was 1196.6 mg, with responders having a lower mean cumulative dose compared with nonresponders (1051.5 mg vs 1673.1 mg, respectively).
Every patient experienced at least one nonserious AE, with 13% considered related/probably related to prednisone, 26% to tocilizumab, and 2% to both medications.
Serious AEs occurred among 13% of participants, including septic olecranon bursitis, diverticulitis, fragility fracture, and cholecystitis. No GCA-related visual manifestations occurred during the treatment phase.
The small sample size and lack of a control group using prednisone were cited as potential study limitations.
Study authors concluded, “[T]he results of this 30-patient open-label trial suggest that tocilizumab in combination with 8 weeks of prednisone might be an efficacious strategy for inducing and maintaining disease remission in patients with giant cell arteritis. Such a strategy could obviate the need for and prevent many of the complications associated with long-term glucocorticoid use.”
Disclosure: One or more of the study authors declared affiliations with biotech, pharmaceutical, and/or device companies. Please see the original reference for a full list of authors’ disclosures.

Facebook Comments